Fall is here.
Through the windows of the angiography office my peripheral vision catches glimpses of falling leaves just behind my computer screen. It's a nice subtle distraction and such a refreshing change of setting from the otherwise rather dull underground windowless facilities of the Radiology department.
What I'm focusing on my screen is new to me. I am writing very short reports now —this time not on chronic suspicious findings, emergency imaging or oncology follow-ups, but on procedures I've actually undertaken myself. Like a true (very amateur) surgeon.
And with less than two weeks of experience, I've concluded the most surgical branch of my field is the coolest.
This is interventional radiology.
And yesterday was probably the best day I’ve had ever since I started working at this Unispital.
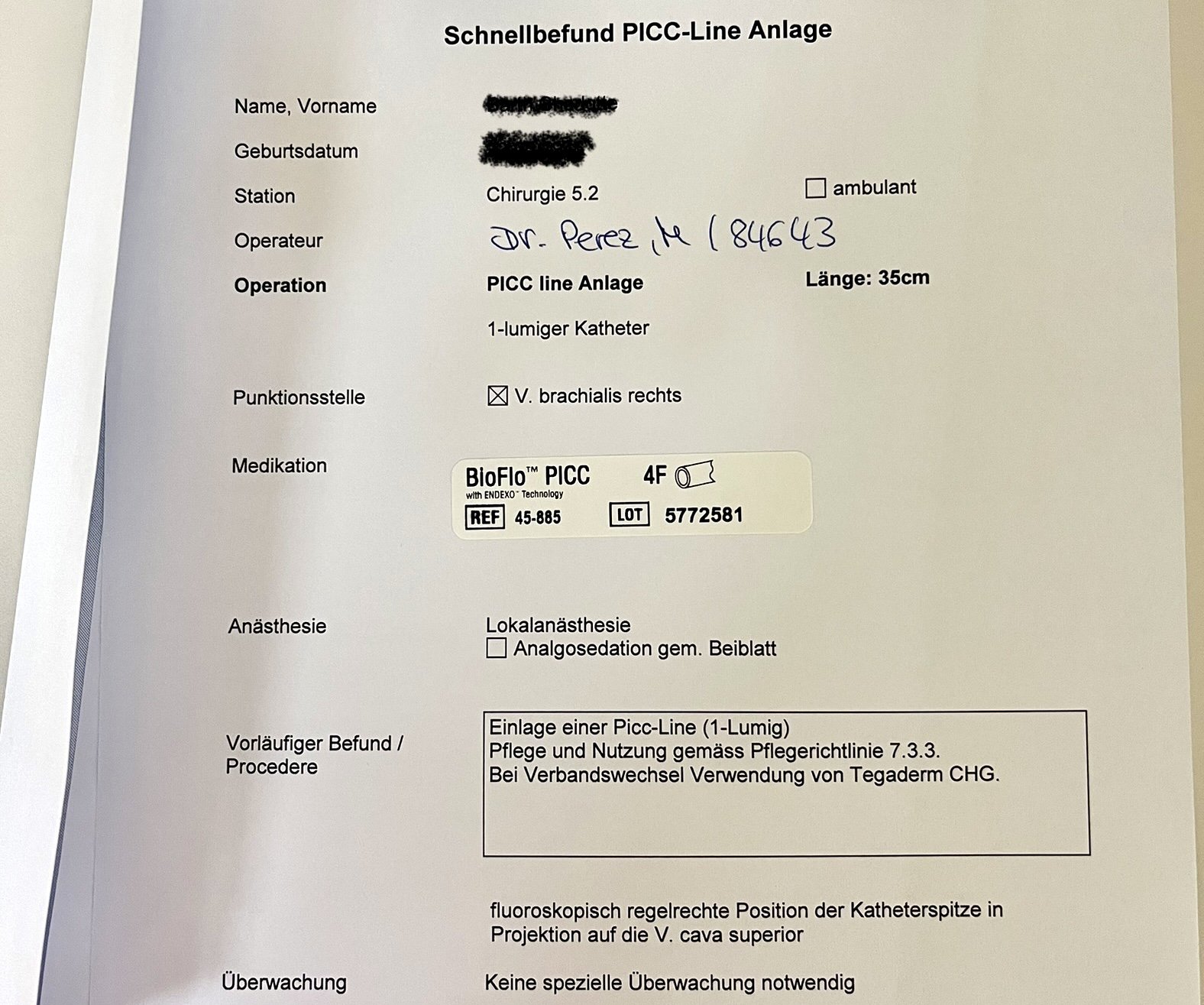
I successfully placed my first PICC-Line on a female patient. In such a way that even she was surprised at the speed of the procedure. “Oh, is it over already? I didn’t feel a thing”. That felt so good.
I’ve always found it strange to pose in front of people as a poised, experienced doctor from day one. And the experience repeats itself with every new rotation. But the fact that it helps so much for both parties to ease into the situation with confidence and trust makes it ok to state things such as “of course, we do this every day” or “it’ll be over very quickly”. Even when I forget to occlude the punctured vein after removing a dilator and there’s a puddle of blood forming on the blue sterile field.
When I know I can finally be successful without any help, it’s really fun to work in sterile conditions, to wear silicone gloves and a surgical gown and to actually talk to the patient in front of me, which is something you barely get to do as a radiologist. I am able to use the ultrasound and fluoroscopy experience gained in the past year at this very same Spital to locate an accessible vein, inject local anesthesia and access the deep vessel with the needle with enough precision not to injure an artery or a nerve. I am able to use a modified Seldinger technique to guide a wire up to the superior vena cava, and to place a catheter all the way up to the heart.
The day continued in this uplifting, reassuring way at the neurology ward, where I helped translate for a Spanish patient, mixing English, German and Spanish over the course of 20 minutes around my fellow international neurointerventional colleagues and the sweet Spanish lady. Delivering good news. The gratitude in her eyes, the kinship, sense of familiarity in her accent and her demeanors, left me fulfilled and happy. Even if I was not the one to coil her aneurysms. Yet.
And then, after work, a more or less unexpected social evening with my newfound favorite medical student, and her friends. We cooked and laughed and talked, and then enjoyed our home-cooked ceviche on a balcony looking out to the rooftops of south Grossbasel to a beautiful sunset, a bit too warm for October.
Finally, while taking a shower last night, I had an epiphany. One of the reasons I wanted to study medicine was to be medically helpful to my family, just like my dad had been to us growing up. Just recently I got to read my own mom’s CT-study, and cousin’s x-rays. It hit me. I already am someone my loved ones can rely on regarding medical issues. And it’s a nice feeling to realize I can already fulfill one of the reasons why I embarked in the journey over a decade ago. Such small things give me the motivation and energy to keep pushing, despite any setbacks, even when times are harder.
I know it’s going to be a lonely winter. It will not be the first, and I'm used to those. But overall, it’s such a good feeling just to have this amount of responsibility and fun at work. To connect with my colleagues. To walk around the hospital and talk to patients. To have many relaxed moments in between tasks to just look through the window and watch the autumn leaves falling, maybe daydreaming a little bit.